More infos about the Withings+ subscription
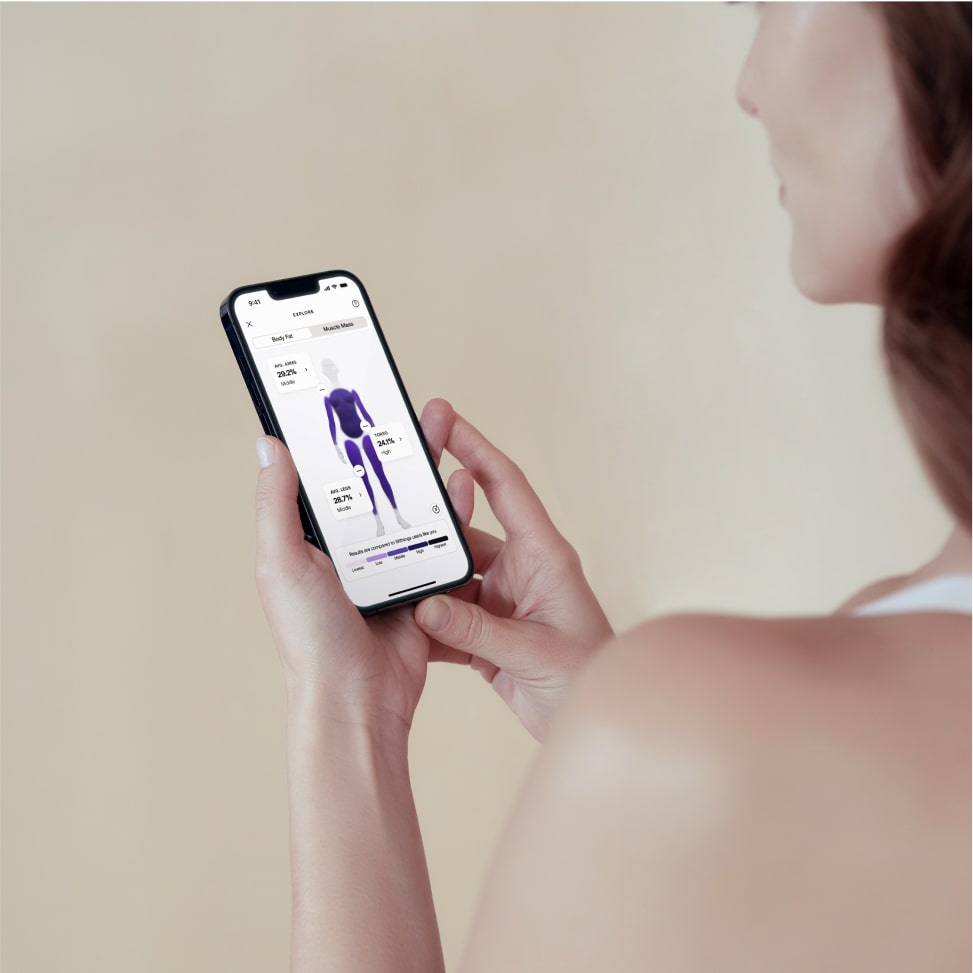
The service Withings+ unlocks an in-app health experience with access to daily engagement support and exclusive content in the areas of sleep, nutrition and activity. With Withings+, you’ll get guided on a daily basis to create a healthy routine that sticks.
Promotional Offers of Withings+ service bundled with a Body Scan health station
For the launch of the Body Scan health station, we offer two introductory subscription (1)(2) plans to the Withings+ service:
Monthly subscription: 3 free months of Withings+, then 9.95€/month (3) Annual subscription: 3 free months of Withings+, then 99,5€/year (corresponding to 8,29€/month) (4) The 3-month trial period starts on the product’s installation using the Withings mobile application.
(1) These introductory offers are not mandatory to use the Body Scan health station. By selecting one of these offers, you agree to conclude a subscription contract with Withings for the Withings+ service with the terms and condition described below. The contract will start upon Body Scan health station installation using the Withings mobile application.
(2) Promotional or introductory offers: we may from time to time offer special promotional offers, plans or subscriptions. Offer eligibility is determined by Withings at its sole discretion and we reserve the right to stop making an offer. It is not possible to combine several promotional offers unless specifically mentioned.
(3) Offer reserved for new Withings+ subscribers only (any person not subscribed to Withings+ service during the last month). Right after the 3-month trial period, the monthly auto-renewal starts and you will be automatically charged 9.95€ (or $9.95 or £9.95) per month. You can unsubscribe at any time. See below for cancellation, termination and usage conditions.
(4) Offer reserved for new Withings+ subscribers only (any person not subscribed to Withings+ service during the last month). Right after the 3-month trial period, the annual auto-renewal starts and you will be automatically charged 99.5€ (or $99.5 or £99.5) per year. You can unsubscribe at any time. See below for cancellation, termination and usage conditions.
Terms and conditions for a Withings+ subscription
General sales conditions and terms of use for Withings digital health products and services are available here: https://www.withings.com/legal/services-terms-and-conditions .
Subscription: Your subscription (also called contract) will continue until terminated. To use the Withings service you must have Internet access and the latest available Withings mobile application, Withings App. Unless you cancel your subscription before your billing date, you authorize us to charge the subscription fee for the next billing cycle to your payment method (see "Cancellation" below). "payment method" means a valid and accepted method of payment.Promotional or introductory offers: we may from time to time offer special promotional offers, plans or subscriptions (“Offers”). Offer eligibility is determined by Withings at its sole discretion and we reserve the right to stop making an Offer. It is not possible to combine several promotional offers unless specifically mentioned.Billing and cancellation Billing Cycle: The subscription fee for the Withings+ service will be charged to your payment method on the specific payment date indicated on the subscription management webpage available on https://healthmate.withings.com. The cycle will be monthly or annual depending on the type of subscription that you chose when you subscribed to the service. In some cases, the payment date may vary if the first attempts of payment fail, if your payment method is not correctly settled, if you change your billing cycle or your paid subscription began on a day not contained in a given month.Payment Methods: To use the Withings service you must provide at least one payment method. Withings will automatically use the payment method used during the initial checkout (credit card, PayPal, Google Pay, Apple Pay…). You can update your payment method at any time (see below). You authorize Withings to charge the payment method associated to your account automatically with or without notice until your subscription is not terminated. For some payment methods, the issuer may charge you certain fees, such as foreign transaction fees or other fees relating to the processing of your payment method. Local tax charges may vary depending on the payment method used. Check with your payment method service provider for details.Uncollected payments: Any uncollected amounts remain due to Withings. If a payment is not successfully settled, due to expiration, insufficient funds, or otherwise, and you do not cancel your account, we may suspend your access to the service until we have successfully charged a valid payment method. In case of payments failure, the next payments will continue to be charged regarding your billing cycle (it does not delay the other due payments).Updating your payment methods: You can update your payment method by going to the subscription management webpage available on https://healthmate.withings.com . At the moment, you can only update your payment method to use credit card method. Following any update, you authorize us to continue to charge the applicable payment method.Cancellation: You can cancel your Withings+ subscription at any time, and you will continue to have access to the service through the end of your billing period. Payments are non-refundable and we do not provide refunds or credits for any partial subscription periods or unused services. To cancel, go to the subscription management webpage available on https://healthmate.withings.com and follow the instructions for cancellation. If you decide to cancel your subscription, the Withings+ service will be discontinued with all included features on the date your subscription ends. Your devices and all their features will continue to function normally.Changes to the Price and Subscription Plans: We may change our subscription plans and the price of our service from time to time; however, any price changes or changes to your subscription plans will apply no earlier than 30 days following notice to you.Right of withdrawal: Legal right of withdrawal: You may withdraw from your subscription order without giving any reason within 14 days from the date the contract start. To comply with the withdrawal deadline, simply send your withdrawal request before the 14-day period expires to our customer support department free of charge: By telephone 0 800 945 713 Online on our customer support department Effect of withdrawal: We will refund all payments we have received from you related to the Withings service. Withdrawal for hardware devices need to be managed separately. We will use the same method of payment that you used for your original order, unless you expressly agree to a different method. In any case, this refund will not cause any additional costs for you. The Withings+ service will be discontinued immediately with all included features. Your devices and all their features will continue to function normally. Acceptable use of the service Right and access: The Withings+ service and any content accessed through the service are for your personal and non-commercial use only and may not be shared with individuals beyond device users. As long as you subscribe to the service, Withings grants you a a limited, non-exclusive, non-transferable, non-sublicensable right to access the service and its related content. You agree not to use the service for public performances.Updates and improvements: The service, including the content library, is regularly updated at our sole discretion at any time with or without notice. In addition, we continually improve or test various aspects of our service, including our user interfaces, promotional features and availability. Those improvements or tests shall not impact your use of the service.Additional software terms: Except as explicitly authorized in these Terms of Use, you agree not to: archive, reproduce, distribute, modify, display, publish, license, create derivative, sale, or use content and information contained on or obtained from or through the Withings service; circumvent, remove, alter, deactivate, degrade, block, obscure or thwart any of the content protections or other elements of the Withings service, including the graphical user interface, any advertising or advertising features, copyright notices, and trademark; use any robot, spider, scraper or other automated means to access the Withings service; reverse engineer, decompile or disassemble, tamper with, or bypass any security associated with any software or other products or processes accessible through the Withings service, whether in whole or in part; use any fraudulent methods like inserting any code or manipulate the content of the Withings service in any way or use any data mining, data gathering or extraction method; Data privacy: We process personal data relating to you during the subscription process. Please refer to our Privacy Policy for more details : https://www.withings.com/fr/en/legal/privacy-policy .Applicable law: These Terms and Conditions shall be governed by the laws of France, without reference to the principles of conflicts of laws. The French courts are competent to judge any dispute arising from these Terms and Conditions.We may terminate or restrict your use of our service if you violate these Terms of Use or are engaged in illegal or fraudulent use of the service.
More infos about the Withings+ subscription
The service Withings+ unlocks an in-app health experience with access to daily engagement support and exclusive content in the areas of sleep, nutrition and activity. With Withings+, you’ll get guided on a daily basis to create a healthy routine that sticks.
Promotional Offers of Withings+ service bundled with a Body Segment
For the launch of the Body Segment, we offer two introductory subscription (1)(2) plans to the Withings+ service:
Monthly subscription: 3 free months of Withings+, then 9.95€/month (3) Annual subscription: 3 free months of Withings+, then 99,5€/year (corresponding to 8,29€/month) (4) The 3-month trial period starts on the product’s installation using the Withings mobile application.
(1) These introductory offers are not mandatory to use the Body Segment. By selecting one of these offers, you agree to conclude a subscription contract with Withings for the Withings+ service with the terms and condition described below. The contract will start upon Body Segment installation using the Withings mobile application.
(2) Promotional or introductory offers: we may from time to time offer special promotional offers, plans or subscriptions. Offer eligibility is determined by Withings at its sole discretion and we reserve the right to stop making an offer. It is not possible to combine several promotional offers unless specifically mentioned.
(3) Offer reserved for new Withings+ subscribers only (any person not subscribed to Withings+ service during the last month). Right after the 3-month trial period, the monthly auto-renewal starts and you will be automatically charged 9.95€ (or $9.95 or £9.95) per month. You can unsubscribe at any time. See below for cancellation, termination and usage conditions.
(4) Offer reserved for new Withings+ subscribers only (any person not subscribed to Withings+ service during the last month). Right after the 3-month trial period, the annual auto-renewal starts and you will be automatically charged 99.5€ (or $99.5 or £99.5) per year. You can unsubscribe at any time. See below for cancellation, termination and usage conditions.
Terms and conditions for a Withings+ subscription
General sales conditions and terms of use for Withings digital health products and services are available here: https://www.withings.com/legal/services-terms-and-conditions .
Subscription: Your subscription (also called contract) will continue until terminated. To use the Withings service you must have Internet access and the latest available Withings mobile application, Withings App. Unless you cancel your subscription before your billing date, you authorize us to charge the subscription fee for the next billing cycle to your payment method (see "Cancellation" below). "payment method" means a valid and accepted method of payment.Promotional or introductory offers: we may from time to time offer special promotional offers, plans or subscriptions (“Offers”). Offer eligibility is determined by Withings at its sole discretion and we reserve the right to stop making an Offer. It is not possible to combine several promotional offers unless specifically mentioned.Billing and cancellation Billing Cycle: The subscription fee for the Withings+ service will be charged to your payment method on the specific payment date indicated on the subscription management webpage available on https://healthmate.withings.com. The cycle will be monthly or annual depending on the type of subscription that you chose when you subscribed to the service. In some cases, the payment date may vary if the first attempts of payment fail, if your payment method is not correctly settled, if you change your billing cycle or your paid subscription began on a day not contained in a given month.Payment Methods: To use the Withings service you must provide at least one payment method. Withings will automatically use the payment method used during the initial checkout (credit card, PayPal, Google Pay, Apple Pay…). You can update your payment method at any time (see below). You authorize Withings to charge the payment method associated to your account automatically with or without notice until your subscription is not terminated. For some payment methods, the issuer may charge you certain fees, such as foreign transaction fees or other fees relating to the processing of your payment method. Local tax charges may vary depending on the payment method used. Check with your payment method service provider for details.Uncollected payments: Any uncollected amounts remain due to Withings. If a payment is not successfully settled, due to expiration, insufficient funds, or otherwise, and you do not cancel your account, we may suspend your access to the service until we have successfully charged a valid payment method. In case of payments failure, the next payments will continue to be charged regarding your billing cycle (it does not delay the other due payments).Updating your payment methods: You can update your payment method by going to the subscription management webpage available on https://healthmate.withings.com . At the moment, you can only update your payment method to use credit card method. Following any update, you authorize us to continue to charge the applicable payment method.Cancellation: You can cancel your Withings+ subscription at any time, and you will continue to have access to the service through the end of your billing period. Payments are non-refundable and we do not provide refunds or credits for any partial subscription periods or unused services. To cancel, go to the subscription management webpage available on https://healthmate.withings.com and follow the instructions for cancellation. If you decide to cancel your subscription, the Withings+ service will be discontinued with all included features on the date your subscription ends. Your devices and all their features will continue to function normally.Changes to the Price and Subscription Plans: We may change our subscription plans and the price of our service from time to time; however, any price changes or changes to your subscription plans will apply no earlier than 30 days following notice to you.Right of withdrawal: Legal right of withdrawal: You may withdraw from your subscription order without giving any reason within 14 days from the date the contract start. To comply with the withdrawal deadline, simply send your withdrawal request before the 14-day period expires to our customer support department free of charge: By telephone 0 800 945 713 Online on our customer support department Effect of withdrawal: We will refund all payments we have received from you related to the Withings service. Withdrawal for hardware devices need to be managed separately. We will use the same method of payment that you used for your original order, unless you expressly agree to a different method. In any case, this refund will not cause any additional costs for you. The Withings+ service will be discontinued immediately with all included features. Your devices and all their features will continue to function normally. Acceptable use of the service Right and access: The Withings+ service and any content accessed through the service are for your personal and non-commercial use only and may not be shared with individuals beyond device users. As long as you subscribe to the service, Withings grants you a a limited, non-exclusive, non-transferable, non-sublicensable right to access the service and its related content. You agree not to use the service for public performances.Updates and improvements: The service, including the content library, is regularly updated at our sole discretion at any time with or without notice. In addition, we continually improve or test various aspects of our service, including our user interfaces, promotional features and availability. Those improvements or tests shall not impact your use of the service.Additional software terms: Except as explicitly authorized in these Terms of Use, you agree not to: archive, reproduce, distribute, modify, display, publish, license, create derivative, sale, or use content and information contained on or obtained from or through the Withings service; circumvent, remove, alter, deactivate, degrade, block, obscure or thwart any of the content protections or other elements of the Withings service, including the graphical user interface, any advertising or advertising features, copyright notices, and trademark; use any robot, spider, scraper or other automated means to access the Withings service; reverse engineer, decompile or disassemble, tamper with, or bypass any security associated with any software or other products or processes accessible through the Withings service, whether in whole or in part; use any fraudulent methods like inserting any code or manipulate the content of the Withings service in any way or use any data mining, data gathering or extraction method; Data privacy: We process personal data relating to you during the subscription process. Please refer to our Privacy Policy for more details : https://www.withings.com/fr/en/legal/privacy-policy .Applicable law: These Terms and Conditions shall be governed by the laws of France, without reference to the principles of conflicts of laws. The French courts are competent to judge any dispute arising from these Terms and Conditions.We may terminate or restrict your use of our service if you violate these Terms of Use or are engaged in illegal or fraudulent use of the service.
More infos about the Withings+ subscription
The service Withings+ unlocks an in-app health experience with access to daily engagement support and exclusive content in the areas of sleep, nutrition and activity. With Withings+, you’ll get guided on a daily basis to create a healthy routine that sticks.
Terms and conditions for a Withings+ subscription
General sales conditions and terms of use for Withings digital health products and services are available here: https://www.withings.com/legal/services-terms-and-conditions .
Subscription: Your subscription (also called contract) will continue until terminated. To use the Withings service you must have Internet access and the latest available Withings mobile application, Withings App. Unless you cancel your subscription before your billing date, you authorize us to charge the subscription fee for the next billing cycle to your payment method (see "Cancellation" below). "payment method" means a valid and accepted method of payment.Promotional or introductory offers: we may from time to time offer special promotional offers, plans or subscriptions (“Offers”). Offer eligibility is determined by Withings at its sole discretion and we reserve the right to stop making an Offer. It is not possible to combine several promotional offers unless specifically mentioned.Billing and cancellation Billing Cycle: The subscription fee for the Withings+ service will be charged to your payment method on the specific payment date indicated on the subscription management webpage available on https://healthmate.withings.com. The cycle will be monthly or annual depending on the type of subscription that you chose when you subscribed to the service. In some cases, the payment date may vary if the first attempts of payment fail, if your payment method is not correctly settled, if you change your billing cycle or your paid subscription began on a day not contained in a given month.Payment Methods: To use the Withings service you must provide at least one payment method. Withings will automatically use the payment method used during the initial checkout (credit card, PayPal, Google Pay, Apple Pay…). You can update your payment method at any time (see below). You authorize Withings to charge the payment method associated to your account automatically with or without notice until your subscription is not terminated. For some payment methods, the issuer may charge you certain fees, such as foreign transaction fees or other fees relating to the processing of your payment method. Local tax charges may vary depending on the payment method used. Check with your payment method service provider for details.Uncollected payments: Any uncollected amounts remain due to Withings. If a payment is not successfully settled, due to expiration, insufficient funds, or otherwise, and you do not cancel your account, we may suspend your access to the service until we have successfully charged a valid payment method. In case of payments failure, the next payments will continue to be charged regarding your billing cycle (it does not delay the other due payments).Updating your payment methods: You can update your payment method by going to the subscription management webpage available on https://healthmate.withings.com . At the moment, you can only update your payment method to use credit card method. Following any update, you authorize us to continue to charge the applicable payment method.Cancellation: You can cancel your Withings+ subscription at any time, and you will continue to have access to the service through the end of your billing period. Payments are non-refundable and we do not provide refunds or credits for any partial subscription periods or unused services. To cancel, go to the subscription management webpage available on https://healthmate.withings.com and follow the instructions for cancellation. If you decide to cancel your subscription, the Withings+ service will be discontinued with all included features on the date your subscription ends. Your devices and all their features will continue to function normally.Changes to the Price and Subscription Plans: We may change our subscription plans and the price of our service from time to time; however, any price changes or changes to your subscription plans will apply no earlier than 30 days following notice to you.Right of withdrawal: Legal right of withdrawal: You may withdraw from your subscription order without giving any reason within 14 days from the date the contract start. To comply with the withdrawal deadline, simply send your withdrawal request before the 14-day period expires to our customer support department free of charge: By telephone 0 800 945 713 Online on our customer support department Effect of withdrawal: We will refund all payments we have received from you related to the Withings service. Withdrawal for hardware devices need to be managed separately. We will use the same method of payment that you used for your original order, unless you expressly agree to a different method. In any case, this refund will not cause any additional costs for you. The Withings+ service will be discontinued immediately with all included features. Your devices and all their features will continue to function normally. Acceptable use of the service Right and access: The Withings+ service and any content accessed through the service are for your personal and non-commercial use only and may not be shared with individuals beyond device users. As long as you subscribe to the service, Withings grants you a a limited, non-exclusive, non-transferable, non-sublicensable right to access the service and its related content. You agree not to use the service for public performances.Updates and improvements: The service, including the content library, is regularly updated at our sole discretion at any time with or without notice. In addition, we continually improve or test various aspects of our service, including our user interfaces, promotional features and availability. Those improvements or tests shall not impact your use of the service.Additional software terms: Except as explicitly authorized in these Terms of Use, you agree not to: archive, reproduce, distribute, modify, display, publish, license, create derivative, sale, or use content and information contained on or obtained from or through the Withings service; circumvent, remove, alter, deactivate, degrade, block, obscure or thwart any of the content protections or other elements of the Withings service, including the graphical user interface, any advertising or advertising features, copyright notices, and trademark; use any robot, spider, scraper or other automated means to access the Withings service; reverse engineer, decompile or disassemble, tamper with, or bypass any security associated with any software or other products or processes accessible through the Withings service, whether in whole or in part; use any fraudulent methods like inserting any code or manipulate the content of the Withings service in any way or use any data mining, data gathering or extraction method; Data privacy: We process personal data relating to you during the subscription process. Please refer to our Privacy Policy for more details : https://www.withings.com/fr/en/legal/privacy-policy .Applicable law: These Terms and Conditions shall be governed by the laws of France, without reference to the principles of conflicts of laws. The French courts are competent to judge any dispute arising from these Terms and Conditions.We may terminate or restrict your use of our service if you violate these Terms of Use or are engaged in illegal or fraudulent use of the service.
More infos about the Withings+ subscription
The service Withings+ unlocks an in-app health experience with access to daily engagement support and exclusive content in the areas of sleep, nutrition and activity. With Withings+, you’ll get guided on a daily basis to create a healthy routine that sticks.
Terms and conditions for a Withings+ subscription
General sales conditions and terms of use for Withings digital health products and services are available here: https://www.withings.com/legal/services-terms-and-conditions .
Subscription: Your subscription (also called contract) will continue until terminated. To use the Withings service you must have Internet access and the latest available Withings mobile application, Withings App. Unless you cancel your subscription before your billing date, you authorize us to charge the subscription fee for the next billing cycle to your payment method (see "Cancellation" below). "payment method" means a valid and accepted method of payment.Promotional or introductory offers: we may from time to time offer special promotional offers, plans or subscriptions (“Offers”). Offer eligibility is determined by Withings at its sole discretion and we reserve the right to stop making an Offer. It is not possible to combine several promotional offers unless specifically mentioned.Billing and cancellation Billing Cycle: The subscription fee for the Withings+ service will be charged to your payment method on the specific payment date indicated on the subscription management webpage available on https://healthmate.withings.com. The cycle will be monthly or annual depending on the type of subscription that you chose when you subscribed to the service. In some cases, the payment date may vary if the first attempts of payment fail, if your payment method is not correctly settled, if you change your billing cycle or your paid subscription began on a day not contained in a given month.Payment Methods: To use the Withings service you must provide at least one payment method. Withings will automatically use the payment method used during the initial checkout (credit card, PayPal, Google Pay, Apple Pay…). You can update your payment method at any time (see below). You authorize Withings to charge the payment method associated to your account automatically with or without notice until your subscription is not terminated. For some payment methods, the issuer may charge you certain fees, such as foreign transaction fees or other fees relating to the processing of your payment method. Local tax charges may vary depending on the payment method used. Check with your payment method service provider for details.Uncollected payments: Any uncollected amounts remain due to Withings. If a payment is not successfully settled, due to expiration, insufficient funds, or otherwise, and you do not cancel your account, we may suspend your access to the service until we have successfully charged a valid payment method. In case of payments failure, the next payments will continue to be charged regarding your billing cycle (it does not delay the other due payments).Updating your payment methods: You can update your payment method by going to the subscription management webpage available on https://healthmate.withings.com . At the moment, you can only update your payment method to use credit card method. Following any update, you authorize us to continue to charge the applicable payment method.Cancellation: You can cancel your Withings+ subscription at any time, and you will continue to have access to the service through the end of your billing period. Payments are non-refundable and we do not provide refunds or credits for any partial subscription periods or unused services. To cancel, go to the subscription management webpage available on https://healthmate.withings.com and follow the instructions for cancellation. If you decide to cancel your subscription, the Withings+ service will be discontinued with all included features on the date your subscription ends. Your devices and all their features will continue to function normally.Changes to the Price and Subscription Plans: We may change our subscription plans and the price of our service from time to time; however, any price changes or changes to your subscription plans will apply no earlier than 30 days following notice to you.Right of withdrawal: Legal right of withdrawal: You may withdraw from your subscription order without giving any reason within 14 days from the date the contract start. To comply with the withdrawal deadline, simply send your withdrawal request before the 14-day period expires to our customer support department free of charge: By telephone 0 800 945 713 Online on our customer support department Effect of withdrawal: We will refund all payments we have received from you related to the Withings service. Withdrawal for hardware devices need to be managed separately. We will use the same method of payment that you used for your original order, unless you expressly agree to a different method. In any case, this refund will not cause any additional costs for you. The Withings+ service will be discontinued immediately with all included features. Your devices and all their features will continue to function normally. Acceptable use of the service Right and access: The Withings+ service and any content accessed through the service are for your personal and non-commercial use only and may not be shared with individuals beyond device users. As long as you subscribe to the service, Withings grants you a a limited, non-exclusive, non-transferable, non-sublicensable right to access the service and its related content. You agree not to use the service for public performances.Updates and improvements: The service, including the content library, is regularly updated at our sole discretion at any time with or without notice. In addition, we continually improve or test various aspects of our service, including our user interfaces, promotional features and availability. Those improvements or tests shall not impact your use of the service.Additional software terms: Except as explicitly authorized in these Terms of Use, you agree not to: archive, reproduce, distribute, modify, display, publish, license, create derivative, sale, or use content and information contained on or obtained from or through the Withings service; circumvent, remove, alter, deactivate, degrade, block, obscure or thwart any of the content protections or other elements of the Withings service, including the graphical user interface, any advertising or advertising features, copyright notices, and trademark; use any robot, spider, scraper or other automated means to access the Withings service; reverse engineer, decompile or disassemble, tamper with, or bypass any security associated with any software or other products or processes accessible through the Withings service, whether in whole or in part; use any fraudulent methods like inserting any code or manipulate the content of the Withings service in any way or use any data mining, data gathering or extraction method; Data privacy: We process personal data relating to you during the subscription process. Please refer to our Privacy Policy for more details : https://www.withings.com/fr/en/legal/privacy-policy .Applicable law: These Terms and Conditions shall be governed by the laws of France, without reference to the principles of conflicts of laws. The French courts are competent to judge any dispute arising from these Terms and Conditions.We may terminate or restrict your use of our service if you violate these Terms of Use or are engaged in illegal or fraudulent use of the service.
More infos about the Withings+ subscription
The service Withings+ unlocks an in-app health experience with access to daily engagement support and exclusive content in the areas of sleep, nutrition and activity. With Withings+, you’ll get guided on a daily basis to create a healthy routine that sticks.
Terms and conditions for a Withings+ subscription
General sales conditions and terms of use for Withings digital health products and services are available here: https://www.withings.com/legal/services-terms-and-conditions .
Subscription: Your subscription (also called contract) will continue until terminated. To use the Withings service you must have Internet access and the latest available Withings mobile application, Withings App. Unless you cancel your subscription before your billing date, you authorize us to charge the subscription fee for the next billing cycle to your payment method (see "Cancellation" below). "payment method" means a valid and accepted method of payment.Promotional or introductory offers: we may from time to time offer special promotional offers, plans or subscriptions (“Offers”). Offer eligibility is determined by Withings at its sole discretion and we reserve the right to stop making an Offer. It is not possible to combine several promotional offers unless specifically mentioned.Billing and cancellation Billing Cycle: The subscription fee for the Withings+ service will be charged to your payment method on the specific payment date indicated on the subscription management webpage available on https://healthmate.withings.com. The cycle will be monthly or annual depending on the type of subscription that you chose when you subscribed to the service. In some cases, the payment date may vary if the first attempts of payment fail, if your payment method is not correctly settled, if you change your billing cycle or your paid subscription began on a day not contained in a given month.Payment Methods: To use the Withings service you must provide at least one payment method. Withings will automatically use the payment method used during the initial checkout (credit card, PayPal, Google Pay, Apple Pay…). You can update your payment method at any time (see below). You authorize Withings to charge the payment method associated to your account automatically with or without notice until your subscription is not terminated. For some payment methods, the issuer may charge you certain fees, such as foreign transaction fees or other fees relating to the processing of your payment method. Local tax charges may vary depending on the payment method used. Check with your payment method service provider for details.Uncollected payments: Any uncollected amounts remain due to Withings. If a payment is not successfully settled, due to expiration, insufficient funds, or otherwise, and you do not cancel your account, we may suspend your access to the service until we have successfully charged a valid payment method. In case of payments failure, the next payments will continue to be charged regarding your billing cycle (it does not delay the other due payments).Updating your payment methods: You can update your payment method by going to the subscription management webpage available on https://healthmate.withings.com . At the moment, you can only update your payment method to use credit card method. Following any update, you authorize us to continue to charge the applicable payment method.Cancellation: You can cancel your Withings+ subscription at any time, and you will continue to have access to the service through the end of your billing period. Payments are non-refundable and we do not provide refunds or credits for any partial subscription periods or unused services. To cancel, go to the subscription management webpage available on https://healthmate.withings.com and follow the instructions for cancellation. If you decide to cancel your subscription, the Withings+ service will be discontinued with all included features on the date your subscription ends. Your devices and all their features will continue to function normally.Changes to the Price and Subscription Plans: We may change our subscription plans and the price of our service from time to time; however, any price changes or changes to your subscription plans will apply no earlier than 30 days following notice to you.Right of withdrawal: Legal right of withdrawal: You may withdraw from your subscription order without giving any reason within 14 days from the date the contract start. To comply with the withdrawal deadline, simply send your withdrawal request before the 14-day period expires to our customer support department free of charge: By telephone 0 800 945 713 Online on our customer support department Effect of withdrawal: We will refund all payments we have received from you related to the Withings service. Withdrawal for hardware devices need to be managed separately. We will use the same method of payment that you used for your original order, unless you expressly agree to a different method. In any case, this refund will not cause any additional costs for you. The Withings+ service will be discontinued immediately with all included features. Your devices and all their features will continue to function normally. Acceptable use of the service Right and access: The Withings+ service and any content accessed through the service are for your personal and non-commercial use only and may not be shared with individuals beyond device users. As long as you subscribe to the service, Withings grants you a a limited, non-exclusive, non-transferable, non-sublicensable right to access the service and its related content. You agree not to use the service for public performances.Updates and improvements: The service, including the content library, is regularly updated at our sole discretion at any time with or without notice. In addition, we continually improve or test various aspects of our service, including our user interfaces, promotional features and availability. Those improvements or tests shall not impact your use of the service.Additional software terms: Except as explicitly authorized in these Terms of Use, you agree not to: archive, reproduce, distribute, modify, display, publish, license, create derivative, sale, or use content and information contained on or obtained from or through the Withings service; circumvent, remove, alter, deactivate, degrade, block, obscure or thwart any of the content protections or other elements of the Withings service, including the graphical user interface, any advertising or advertising features, copyright notices, and trademark; use any robot, spider, scraper or other automated means to access the Withings service; reverse engineer, decompile or disassemble, tamper with, or bypass any security associated with any software or other products or processes accessible through the Withings service, whether in whole or in part; use any fraudulent methods like inserting any code or manipulate the content of the Withings service in any way or use any data mining, data gathering or extraction method; Data privacy: We process personal data relating to you during the subscription process. Please refer to our Privacy Policy for more details : https://www.withings.com/fr/en/legal/privacy-policy .Applicable law: These Terms and Conditions shall be governed by the laws of France, without reference to the principles of conflicts of laws. The French courts are competent to judge any dispute arising from these Terms and Conditions.We may terminate or restrict your use of our service if you violate these Terms of Use or are engaged in illegal or fraudulent use of the service.
More infos about the Withings+ subscription
The service Withings+ unlocks an in-app health experience with access to daily engagement support and exclusive content in the areas of sleep, nutrition and activity. With Withings+, you’ll get guided on a daily basis to create a healthy routine that sticks.
Promotional Offers of Withings+ service bundled with a Scanwatch Nova
For the launch of Scanwatch Nova, we offer two introductory subscription (1)(2) plans to the Withings+ service:
Monthly subscription: 3 free months of Withings+, then 9.95€/month (3) Annual subscription: 3 free months of Withings+, then 99,5€/year (corresponding to 8,29€/month) (4) The 3-month trial period starts on the product’s installation using the Withings mobile application.
(1) These introductory offers are not mandatory to use the Scanwatch Nova. By selecting one of these offers, you agree to conclude a subscription contract with Withings for the Withings+ service with the terms and condition described below. The contract will start upon Scanwatch Nova installation using the Withings mobile application.
(2) Promotional or introductory offers: we may from time to time offer special promotional offers, plans or subscriptions. Offer eligibility is determined by Withings at its sole discretion and we reserve the right to stop making an offer. It is not possible to combine several promotional offers unless specifically mentioned.
(3) Offer reserved for new Withings+ subscribers only (any person not subscribed to Withings+ service during the last month). Right after the 3-month trial period, the monthly auto-renewal starts and you will be automatically charged 9.95€ (or $9.95 or £9.95) per month. You can unsubscribe at any time. See below for cancellation, termination and usage conditions.
(4) Offer reserved for new Withings+ subscribers only (any person not subscribed to Withings+ service during the last month). Right after the 3-month trial period, the annual auto-renewal starts and you will be automatically charged 99.5€ (or $99.5 or £99.5) per year. You can unsubscribe at any time. See below for cancellation, termination and usage conditions.
Terms and conditions for a Withings+ subscription
General sales conditions and terms of use for Withings digital health products and services are available here: https://www.withings.com/legal/services-terms-and-conditions .
Subscription: Your subscription (also called contract) will continue until terminated. To use the Withings service you must have Internet access and the latest available Withings mobile application, Withings App. Unless you cancel your subscription before your billing date, you authorize us to charge the subscription fee for the next billing cycle to your payment method (see "Cancellation" below). "payment method" means a valid and accepted method of payment.Promotional or introductory offers: we may from time to time offer special promotional offers, plans or subscriptions (“Offers”). Offer eligibility is determined by Withings at its sole discretion and we reserve the right to stop making an Offer. It is not possible to combine several promotional offers unless specifically mentioned.Billing and cancellation Billing Cycle: The subscription fee for the Withings+ service will be charged to your payment method on the specific payment date indicated on the subscription management webpage available on https://healthmate.withings.com. The cycle will be monthly or annual depending on the type of subscription that you chose when you subscribed to the service. In some cases, the payment date may vary if the first attempts of payment fail, if your payment method is not correctly settled, if you change your billing cycle or your paid subscription began on a day not contained in a given month.Payment Methods: To use the Withings service you must provide at least one payment method. Withings will automatically use the payment method used during the initial checkout (credit card, PayPal, Google Pay, Apple Pay…). You can update your payment method at any time (see below). You authorize Withings to charge the payment method associated to your account automatically with or without notice until your subscription is not terminated. For some payment methods, the issuer may charge you certain fees, such as foreign transaction fees or other fees relating to the processing of your payment method. Local tax charges may vary depending on the payment method used. Check with your payment method service provider for details.Uncollected payments: Any uncollected amounts remain due to Withings. If a payment is not successfully settled, due to expiration, insufficient funds, or otherwise, and you do not cancel your account, we may suspend your access to the service until we have successfully charged a valid payment method. In case of payments failure, the next payments will continue to be charged regarding your billing cycle (it does not delay the other due payments).Updating your payment methods: You can update your payment method by going to the subscription management webpage available on https://healthmate.withings.com . At the moment, you can only update your payment method to use credit card method. Following any update, you authorize us to continue to charge the applicable payment method.Cancellation: You can cancel your Withings+ subscription at any time, and you will continue to have access to the service through the end of your billing period. Payments are non-refundable and we do not provide refunds or credits for any partial subscription periods or unused services. To cancel, go to the subscription management webpage available on https://healthmate.withings.com and follow the instructions for cancellation. If you decide to cancel your subscription, the Withings+ service will be discontinued with all included features on the date your subscription ends. Your devices and all their features will continue to function normally.Changes to the Price and Subscription Plans: We may change our subscription plans and the price of our service from time to time; however, any price changes or changes to your subscription plans will apply no earlier than 30 days following notice to you.Right of withdrawal: Legal right of withdrawal: You may withdraw from your subscription order without giving any reason within 14 days from the date the contract start. To comply with the withdrawal deadline, simply send your withdrawal request before the 14-day period expires to our customer support department free of charge: By telephone 0 800 945 713 Online on our customer support department Effect of withdrawal: We will refund all payments we have received from you related to the Withings service. Withdrawal for hardware devices need to be managed separately. We will use the same method of payment that you used for your original order, unless you expressly agree to a different method. In any case, this refund will not cause any additional costs for you. The Withings+ service will be discontinued immediately with all included features. Your devices and all their features will continue to function normally. Acceptable use of the service Right and access: The Withings+ service and any content accessed through the service are for your personal and non-commercial use only and may not be shared with individuals beyond device users. As long as you subscribe to the service, Withings grants you a a limited, non-exclusive, non-transferable, non-sublicensable right to access the service and its related content. You agree not to use the service for public performances.Updates and improvements: The service, including the content library, is regularly updated at our sole discretion at any time with or without notice. In addition, we continually improve or test various aspects of our service, including our user interfaces, promotional features and availability. Those improvements or tests shall not impact your use of the service.Additional software terms: Except as explicitly authorized in these Terms of Use, you agree not to: archive, reproduce, distribute, modify, display, publish, license, create derivative, sale, or use content and information contained on or obtained from or through the Withings service; circumvent, remove, alter, deactivate, degrade, block, obscure or thwart any of the content protections or other elements of the Withings service, including the graphical user interface, any advertising or advertising features, copyright notices, and trademark; use any robot, spider, scraper or other automated means to access the Withings service; reverse engineer, decompile or disassemble, tamper with, or bypass any security associated with any software or other products or processes accessible through the Withings service, whether in whole or in part; use any fraudulent methods like inserting any code or manipulate the content of the Withings service in any way or use any data mining, data gathering or extraction method; Data privacy: We process personal data relating to you during the subscription process. Please refer to our Privacy Policy for more details : https://www.withings.com/fr/en/legal/privacy-policy .Applicable law: These Terms and Conditions shall be governed by the laws of France, without reference to the principles of conflicts of laws. The French courts are competent to judge any dispute arising from these Terms and Conditions.We may terminate or restrict your use of our service if you violate these Terms of Use or are engaged in illegal or fraudulent use of the service.
More infos about the Withings+ subscription
The service Withings+ unlocks an in-app health experience with access to daily engagement support and exclusive content in the areas of sleep, nutrition and activity. With Withings+, you’ll get guided on a daily basis to create a healthy routine that sticks.
Promotional Offers of Withings+ service bundled with a Scanwatch 2
For the launch of Scanwatch 2, we offer two introductory subscription (1)(2) plans to the Withings+ service:
Monthly subscription: 3 free months of Withings+, then 9.95€/month (3) Annual subscription: 3 free months of Withings+, then 99,5€/year (corresponding to 8,29€/month) (4) The 3-month trial period starts on the product’s installation using the Withings mobile application.
(1) These introductory offers are not mandatory to use the Scanwatch 2. By selecting one of these offers, you agree to conclude a subscription contract with Withings for the Withings+ service with the terms and condition described below. The contract will start upon Scanwatch 2 installation using the Withings mobile application.
(2) Promotional or introductory offers: we may from time to time offer special promotional offers, plans or subscriptions. Offer eligibility is determined by Withings at its sole discretion and we reserve the right to stop making an offer. It is not possible to combine several promotional offers unless specifically mentioned.
(3) Offer reserved for new Withings+ subscribers only (any person not subscribed to Withings+ service during the last month). Right after the 3-month trial period, the monthly auto-renewal starts and you will be automatically charged 9.95€ (or $9.95 or £9.95) per month. You can unsubscribe at any time. See below for cancellation, termination and usage conditions.
(4) Offer reserved for new Withings+ subscribers only (any person not subscribed to Withings+ service during the last month). Right after the 3-month trial period, the annual auto-renewal starts and you will be automatically charged 99.5€ (or $99.5 or £99.5) per year. You can unsubscribe at any time. See below for cancellation, termination and usage conditions.
Terms and conditions for a Withings+ subscription
General sales conditions and terms of use for Withings digital health products and services are available here: https://www.withings.com/legal/services-terms-and-conditions .
Subscription: Your subscription (also called contract) will continue until terminated. To use the Withings service you must have Internet access and the latest available Withings mobile application, Withings App. Unless you cancel your subscription before your billing date, you authorize us to charge the subscription fee for the next billing cycle to your payment method (see "Cancellation" below). "payment method" means a valid and accepted method of payment.Promotional or introductory offers: we may from time to time offer special promotional offers, plans or subscriptions (“Offers”). Offer eligibility is determined by Withings at its sole discretion and we reserve the right to stop making an Offer. It is not possible to combine several promotional offers unless specifically mentioned.Billing and cancellation Billing Cycle: The subscription fee for the Withings+ service will be charged to your payment method on the specific payment date indicated on the subscription management webpage available on https://healthmate.withings.com. The cycle will be monthly or annual depending on the type of subscription that you chose when you subscribed to the service. In some cases, the payment date may vary if the first attempts of payment fail, if your payment method is not correctly settled, if you change your billing cycle or your paid subscription began on a day not contained in a given month.Payment Methods: To use the Withings service you must provide at least one payment method. Withings will automatically use the payment method used during the initial checkout (credit card, PayPal, Google Pay, Apple Pay…). You can update your payment method at any time (see below). You authorize Withings to charge the payment method associated to your account automatically with or without notice until your subscription is not terminated. For some payment methods, the issuer may charge you certain fees, such as foreign transaction fees or other fees relating to the processing of your payment method. Local tax charges may vary depending on the payment method used. Check with your payment method service provider for details.Uncollected payments: Any uncollected amounts remain due to Withings. If a payment is not successfully settled, due to expiration, insufficient funds, or otherwise, and you do not cancel your account, we may suspend your access to the service until we have successfully charged a valid payment method. In case of payments failure, the next payments will continue to be charged regarding your billing cycle (it does not delay the other due payments).Updating your payment methods: You can update your payment method by going to the subscription management webpage available on https://healthmate.withings.com . At the moment, you can only update your payment method to use credit card method. Following any update, you authorize us to continue to charge the applicable payment method.Cancellation: You can cancel your Withings+ subscription at any time, and you will continue to have access to the service through the end of your billing period. Payments are non-refundable and we do not provide refunds or credits for any partial subscription periods or unused services. To cancel, go to the subscription management webpage available on https://healthmate.withings.com and follow the instructions for cancellation. If you decide to cancel your subscription, the Withings+ service will be discontinued with all included features on the date your subscription ends. Your devices and all their features will continue to function normally.Changes to the Price and Subscription Plans: We may change our subscription plans and the price of our service from time to time; however, any price changes or changes to your subscription plans will apply no earlier than 30 days following notice to you.Right of withdrawal: Legal right of withdrawal: You may withdraw from your subscription order without giving any reason within 14 days from the date the contract start. To comply with the withdrawal deadline, simply send your withdrawal request before the 14-day period expires to our customer support department free of charge: By telephone 0 800 945 713 Online on our customer support department Effect of withdrawal: We will refund all payments we have received from you related to the Withings service. Withdrawal for hardware devices need to be managed separately. We will use the same method of payment that you used for your original order, unless you expressly agree to a different method. In any case, this refund will not cause any additional costs for you. The Withings+ service will be discontinued immediately with all included features. Your devices and all their features will continue to function normally. Acceptable use of the service Right and access: The Withings+ service and any content accessed through the service are for your personal and non-commercial use only and may not be shared with individuals beyond device users. As long as you subscribe to the service, Withings grants you a a limited, non-exclusive, non-transferable, non-sublicensable right to access the service and its related content. You agree not to use the service for public performances.Updates and improvements: The service, including the content library, is regularly updated at our sole discretion at any time with or without notice. In addition, we continually improve or test various aspects of our service, including our user interfaces, promotional features and availability. Those improvements or tests shall not impact your use of the service.Additional software terms: Except as explicitly authorized in these Terms of Use, you agree not to: archive, reproduce, distribute, modify, display, publish, license, create derivative, sale, or use content and information contained on or obtained from or through the Withings service; circumvent, remove, alter, deactivate, degrade, block, obscure or thwart any of the content protections or other elements of the Withings service, including the graphical user interface, any advertising or advertising features, copyright notices, and trademark; use any robot, spider, scraper or other automated means to access the Withings service; reverse engineer, decompile or disassemble, tamper with, or bypass any security associated with any software or other products or processes accessible through the Withings service, whether in whole or in part; use any fraudulent methods like inserting any code or manipulate the content of the Withings service in any way or use any data mining, data gathering or extraction method; Data privacy: We process personal data relating to you during the subscription process. Please refer to our Privacy Policy for more details : https://www.withings.com/fr/en/legal/privacy-policy .Applicable law: These Terms and Conditions shall be governed by the laws of France, without reference to the principles of conflicts of laws. The French courts are competent to judge any dispute arising from these Terms and Conditions.We may terminate or restrict your use of our service if you violate these Terms of Use or are engaged in illegal or fraudulent use of the service.
More infos about the Withings+ subscription
The service Withings+ unlocks an in-app health experience with access to daily engagement support and exclusive content in the areas of sleep, nutrition and activity. With Withings+, you’ll get guided on a daily basis to create a healthy routine that sticks.
Terms and conditions for a Withings+ subscription
General sales conditions and terms of use for Withings digital health products and services are available here: https://www.withings.com/legal/services-terms-and-conditions .
Subscription: Your subscription (also called contract) will continue until terminated. To use the Withings service you must have Internet access and the latest available Withings mobile application, Withings App. Unless you cancel your subscription before your billing date, you authorize us to charge the subscription fee for the next billing cycle to your payment method (see "Cancellation" below). "payment method" means a valid and accepted method of payment.Promotional or introductory offers: we may from time to time offer special promotional offers, plans or subscriptions (“Offers”). Offer eligibility is determined by Withings at its sole discretion and we reserve the right to stop making an Offer. It is not possible to combine several promotional offers unless specifically mentioned.Billing and cancellation Billing Cycle: The subscription fee for the Withings+ service will be charged to your payment method on the specific payment date indicated on the subscription management webpage available on https://healthmate.withings.com. The cycle will be monthly or annual depending on the type of subscription that you chose when you subscribed to the service. In some cases, the payment date may vary if the first attempts of payment fail, if your payment method is not correctly settled, if you change your billing cycle or your paid subscription began on a day not contained in a given month.Payment Methods: To use the Withings service you must provide at least one payment method. Withings will automatically use the payment method used during the initial checkout (credit card, PayPal, Google Pay, Apple Pay…). You can update your payment method at any time (see below). You authorize Withings to charge the payment method associated to your account automatically with or without notice until your subscription is not terminated. For some payment methods, the issuer may charge you certain fees, such as foreign transaction fees or other fees relating to the processing of your payment method. Local tax charges may vary depending on the payment method used. Check with your payment method service provider for details.Uncollected payments: Any uncollected amounts remain due to Withings. If a payment is not successfully settled, due to expiration, insufficient funds, or otherwise, and you do not cancel your account, we may suspend your access to the service until we have successfully charged a valid payment method. In case of payments failure, the next payments will continue to be charged regarding your billing cycle (it does not delay the other due payments).Updating your payment methods: You can update your payment method by going to the subscription management webpage available on https://healthmate.withings.com . At the moment, you can only update your payment method to use credit card method. Following any update, you authorize us to continue to charge the applicable payment method.Cancellation: You can cancel your Withings+ subscription at any time, and you will continue to have access to the service through the end of your billing period. Payments are non-refundable and we do not provide refunds or credits for any partial subscription periods or unused services. To cancel, go to the subscription management webpage available on https://healthmate.withings.com and follow the instructions for cancellation. If you decide to cancel your subscription, the Withings+ service will be discontinued with all included features on the date your subscription ends. Your devices and all their features will continue to function normally.Changes to the Price and Subscription Plans: We may change our subscription plans and the price of our service from time to time; however, any price changes or changes to your subscription plans will apply no earlier than 30 days following notice to you.Right of withdrawal: Legal right of withdrawal: You may withdraw from your subscription order without giving any reason within 14 days from the date the contract start. To comply with the withdrawal deadline, simply send your withdrawal request before the 14-day period expires to our customer support department free of charge: By telephone 0 800 945 713 Online on our customer support department Effect of withdrawal: We will refund all payments we have received from you related to the Withings service. Withdrawal for hardware devices need to be managed separately. We will use the same method of payment that you used for your original order, unless you expressly agree to a different method. In any case, this refund will not cause any additional costs for you. The Withings+ service will be discontinued immediately with all included features. Your devices and all their features will continue to function normally. Acceptable use of the service Right and access: The Withings+ service and any content accessed through the service are for your personal and non-commercial use only and may not be shared with individuals beyond device users. As long as you subscribe to the service, Withings grants you a a limited, non-exclusive, non-transferable, non-sublicensable right to access the service and its related content. You agree not to use the service for public performances.Updates and improvements: The service, including the content library, is regularly updated at our sole discretion at any time with or without notice. In addition, we continually improve or test various aspects of our service, including our user interfaces, promotional features and availability. Those improvements or tests shall not impact your use of the service.Additional software terms: Except as explicitly authorized in these Terms of Use, you agree not to: archive, reproduce, distribute, modify, display, publish, license, create derivative, sale, or use content and information contained on or obtained from or through the Withings service; circumvent, remove, alter, deactivate, degrade, block, obscure or thwart any of the content protections or other elements of the Withings service, including the graphical user interface, any advertising or advertising features, copyright notices, and trademark; use any robot, spider, scraper or other automated means to access the Withings service; reverse engineer, decompile or disassemble, tamper with, or bypass any security associated with any software or other products or processes accessible through the Withings service, whether in whole or in part; use any fraudulent methods like inserting any code or manipulate the content of the Withings service in any way or use any data mining, data gathering or extraction method; Data privacy: We process personal data relating to you during the subscription process. Please refer to our Privacy Policy for more details : https://www.withings.com/fr/en/legal/privacy-policy .Applicable law: These Terms and Conditions shall be governed by the laws of France, without reference to the principles of conflicts of laws. The French courts are competent to judge any dispute arising from these Terms and Conditions.We may terminate or restrict your use of our service if you violate these Terms of Use or are engaged in illegal or fraudulent use of the service.